Why Understanding Periodontal Disease Could Save Your Smile
What is periodontal disease is one of the most important questions you can ask about your oral health. Simply put, periodontal disease is a bacterial infection that attacks the gums and tissues supporting your teeth, potentially leading to tooth loss if left untreated.
Quick Answer:
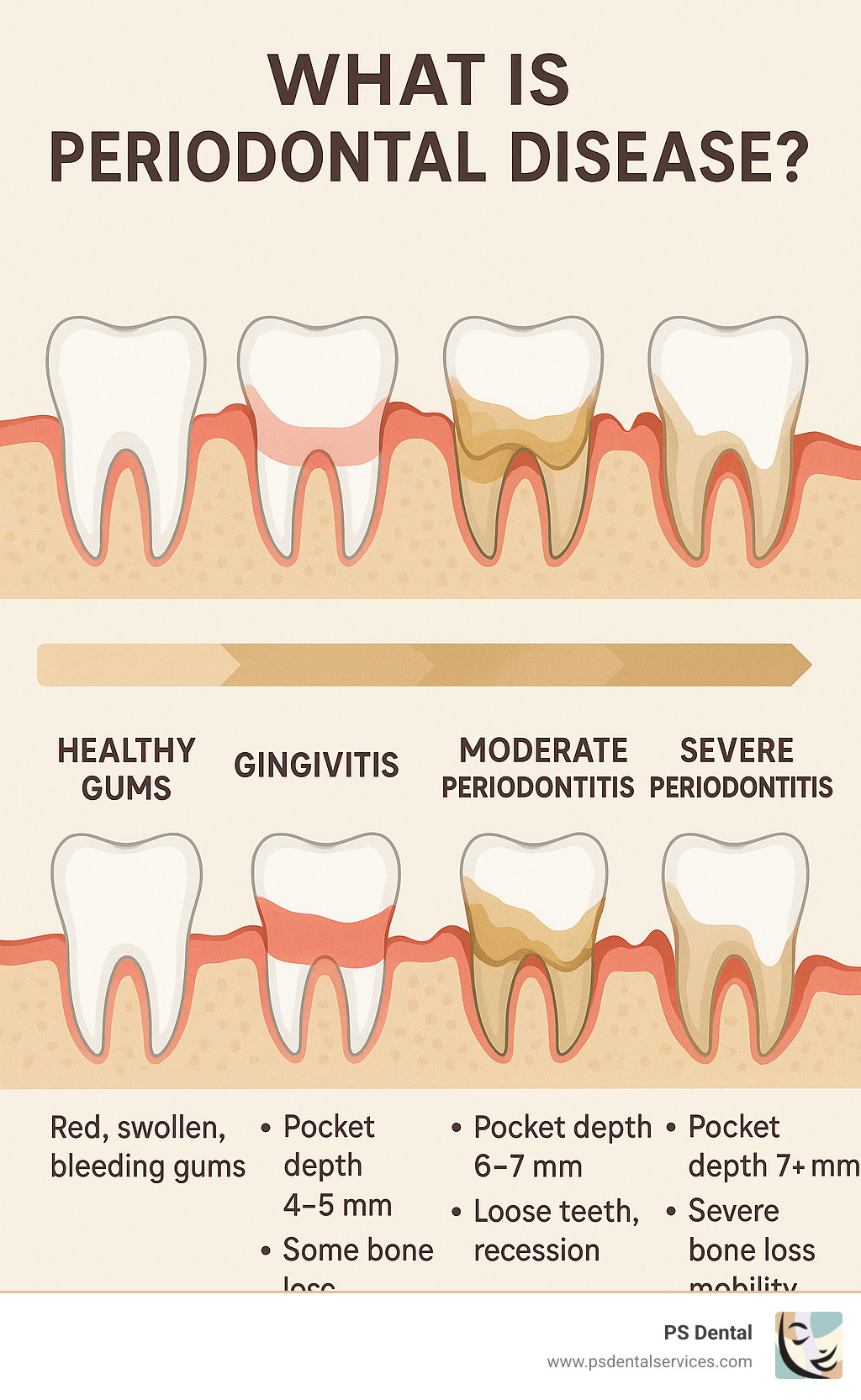
– Gingivitis: Early stage with red, swollen, bleeding gums (reversible)
– Periodontitis: Advanced stage affecting bone and tissue (manageable but not curable)
– Caused by: Plaque buildup, poor oral hygiene, smoking, diabetes, genetics
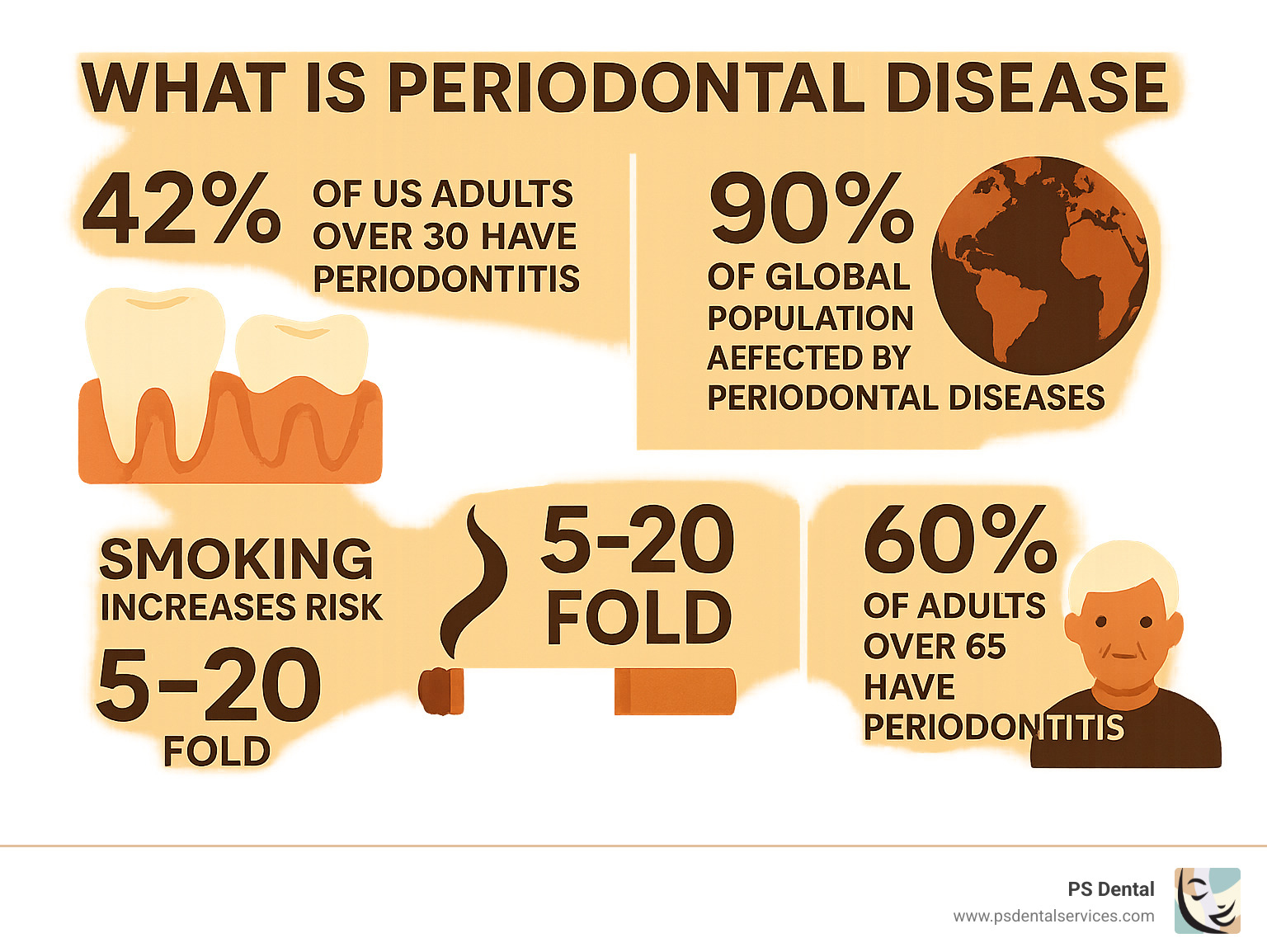
– Affects: About 4 in 10 U.S. adults aged 30+ have some form of periodontitis
The numbers are staggering. Research shows that periodontal diseases affect up to 90% of the global population, making it the most common oral disease worldwide. In the United States alone, approximately 50% of adults currently have some form of gingivitis.
What makes this condition particularly concerning is that it’s often called a “silent disease.” Many people don’t realize they have it until significant damage has already occurred. The progression from healthy gums to advanced periodontal disease happens gradually, starting with simple plaque buildup and eventually leading to bone loss and tooth mobility.
As Dr. Parisa Sepehri, I’ve spent over 30 years helping patients understand and treat periodontal disease, and I’ve seen how early detection and proper care can completely change outcomes.
What is periodontal disease terms explained:
– periodontal disease treatment
– periodontal gum disease treatment cost
What is Periodontal Disease?
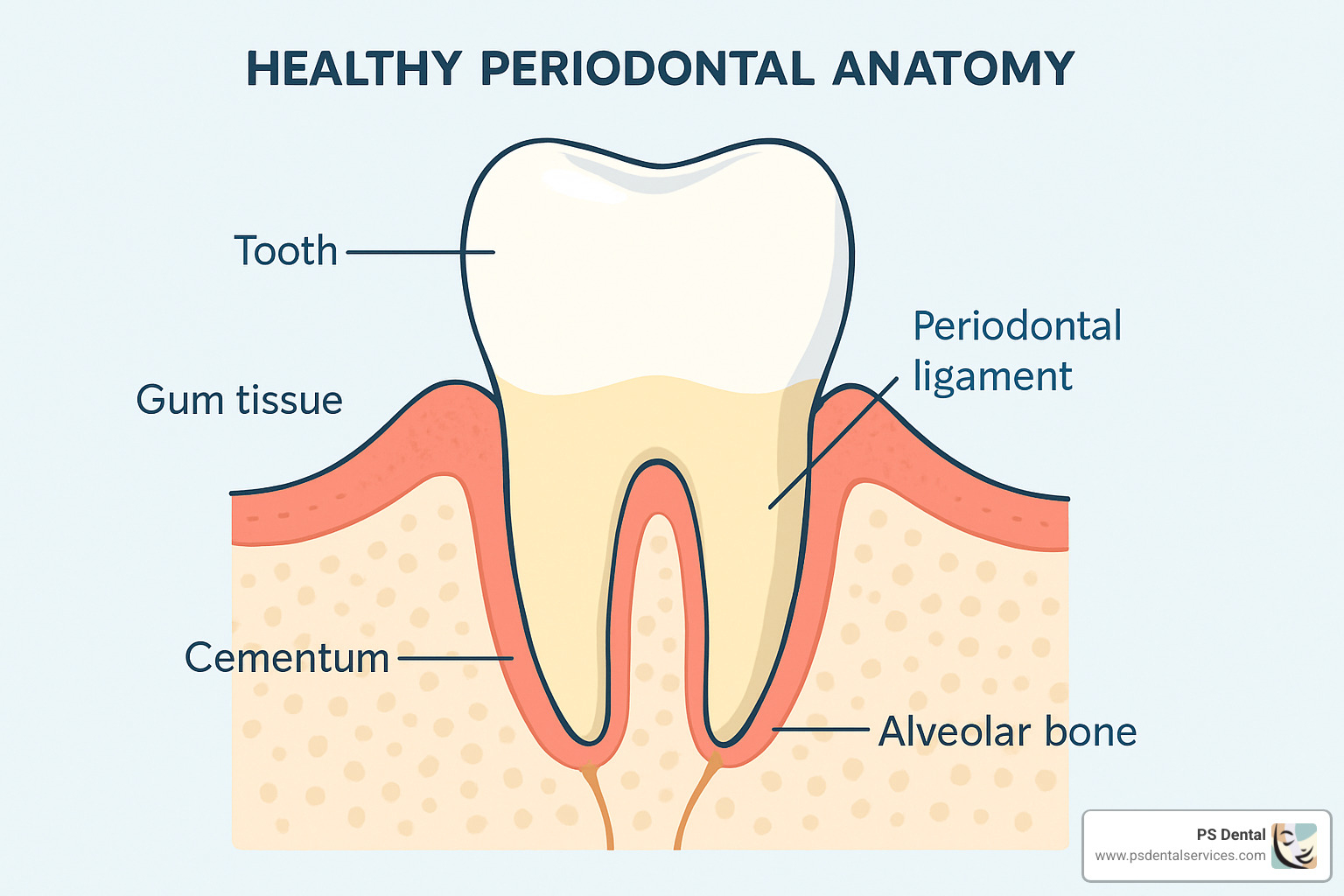
The word “periodontal” literally means “around the tooth,” which gives us a perfect clue about what we’re dealing with. What is periodontal disease at its core? It’s a bacterial infection that targets the periodontium – the group of specialized tissues surrounding and supporting your teeth.
Think of your mouth like a garden. Your teeth are like beautiful flowers, but they need healthy soil and strong roots to thrive. The periodontium includes your gums, the periodontal ligament that connects your tooth to the bone, the cementum covering your tooth roots, and the alveolar bone that holds everything in place.
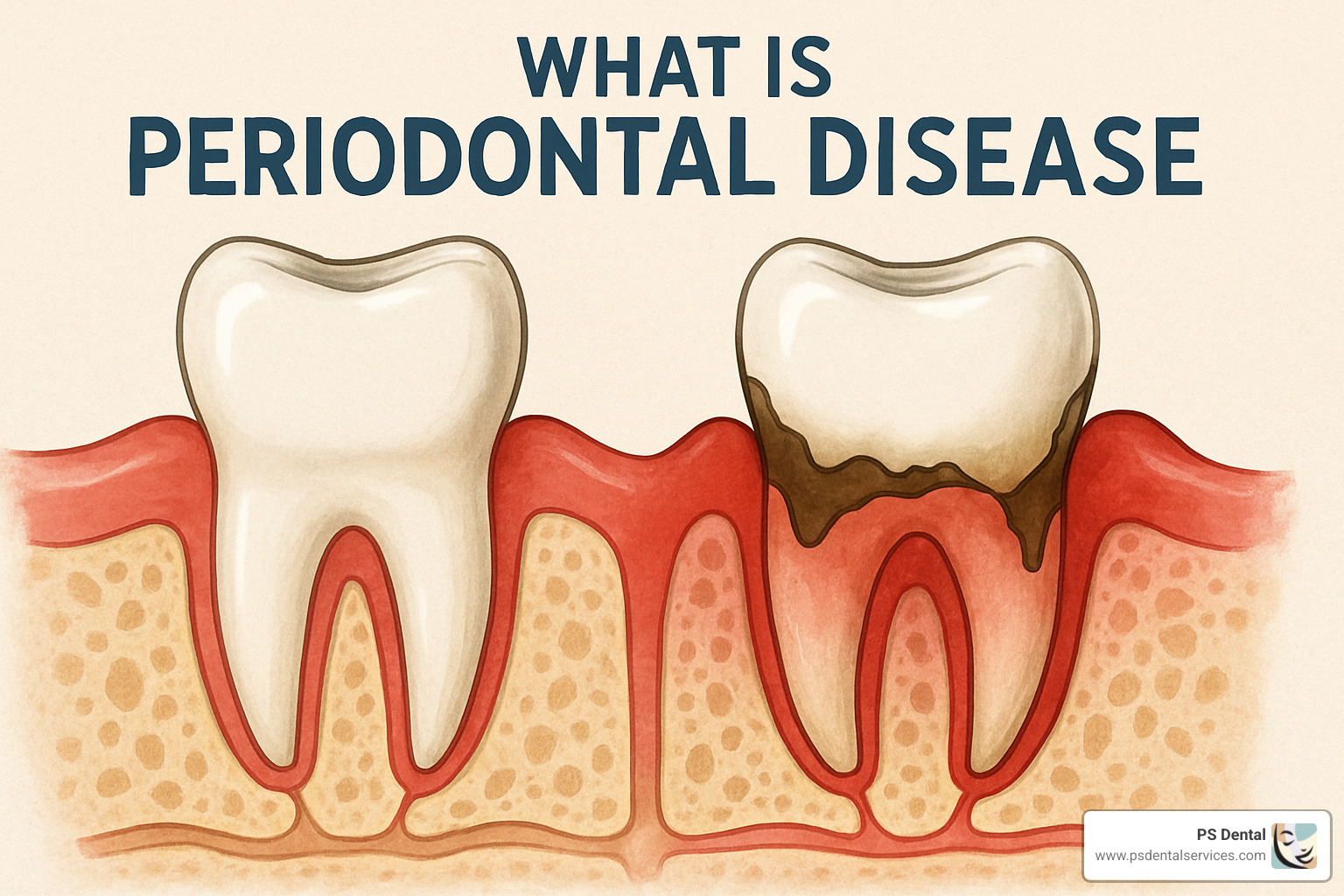
What is periodontal disease becomes clearer when you understand it as a chronic infection caused by bacterial biofilm. This biofilm – basically a sticky community of bacteria we commonly call plaque – contains hundreds of different bacterial species that love to party on your teeth. Unfortunately, their party favors include toxins that irritate your gums.
Your immune system responds with inflammation to fight off these bacterial invaders. But here’s where things get tricky: when this inflammatory response becomes chronic, it can actually start breaking down the very tissues it’s trying to protect.
The disease typically follows a predictable path: healthy gums transform into gingivitis, which can then progress to periodontitis. What makes this particularly sneaky is that each stage can develop without obvious warning signs, especially early on.
Defining “what is periodontal disease” for everyday patients
When patients ask me what is periodontal disease, I like to use simple comparisons they can relate to. Picture your gums as a protective weather seal around each tooth, keeping bacteria and food particles from getting where they shouldn’t be.
When plaque builds up along your gum line, it’s like having dirt and debris constantly rubbing against that seal. The irritation causes inflammation, and you’ve got gingivitis – the earliest stage of periodontal disease.
You might notice your gums bleeding when you brush or floss, looking red and puffy instead of healthy pink, or feeling tender when you eat or clean your teeth. The fantastic news? Gingivitis is completely reversible with good oral hygiene and professional cleanings.
But if we ignore gingivitis, the infection moves below the gum line and begins attacking the bone that anchors your teeth. This is periodontitis, and while we can manage it very effectively, we can’t completely reverse the damage that’s already been done.
Scientific deep dive: what is periodontal disease in clinical terms
From a clinical standpoint, what is periodontal disease involves a destructive battle between bacterial pathogens and your body’s immune system. The condition develops when there’s dysbiosis – essentially, an imbalance where harmful bacteria in your mouth outnumber the good guys.
The main troublemakers include bacteria like Porphyromonas gingivalis, Tannerella forsythia, and Treponema denticola. Scientists call these the “red complex” bacteria because they’re particularly good at causing damage.
Your body fights back by releasing inflammatory mediators that include tumor necrosis factor-alpha, matrix metalloproteinases, and various interleukins. While these are meant to fight the infection, chronic activation creates problems.
The ongoing battle leads to alveolar bone loss, periodontal ligament destruction, and loss of clinical attachment. This creates deeper pockets where more bacteria can hide and multiply, creating a vicious cycle of infection and tissue destruction.
Stages, Causes, Symptoms & Risk Factors
When patients ask me “what is periodontal disease” and how it progresses, I like to explain it as a journey that your gums take. Understanding where you are on this journey helps us determine the best path forward for your oral health.
The dental community uses a sophisticated classification system to track periodontal disease progression. We organize periodontitis into stages I through IV based on how severe the damage is, and grades A through C based on how quickly the disease is moving.
Gingivitis is where everyone’s periodontal story begins if things start going wrong. Your gums become red and swollen, and they might bleed when you brush your teeth. The good news? This is completely reversible with better brushing, flossing, and professional cleaning.
Stage I Periodontitis is when things get more serious. The infection has moved below the gum line and started attacking the bone that holds your teeth in place. Less than 15% of your tooth’s root length is affected. You might notice persistent bad breath or your gums starting to pull back from your teeth.
Stage II Periodontitis shows moderate bone loss between 15-33% of the root length. The pockets around your teeth deepen to 4-5mm (healthy pockets are 1-3mm). Your teeth might start feeling slightly loose, and gum recession becomes more noticeable.
Stage III Periodontitis involves severe bone loss – more than 33% of the root length is affected. The pockets around your teeth are deeper than 6mm. Teeth become noticeably mobile, and you might notice changes in how your teeth fit together when you bite.
Stage IV Periodontitis represents the most advanced stage, where tooth loss becomes likely without aggressive treatment. The bone and tissue destruction is extensive, and teeth may shift position or fall out on their own.
The grading system tells us how fast the disease is progressing. Grade A means slow progression, Grade B indicates moderate progression, while Grade C means rapid progression, often seen in smokers or people with diabetes.
What Actually Causes Periodontal Disease?
The simple answer is plaque – that sticky film of bacteria that forms on your teeth every single day. When you don’t remove plaque through brushing and flossing, it hardens into tartar, which acts like a rough surface that attracts even more bacteria.
But not everyone with plaque develops severe periodontal disease. Several risk factors dramatically increase your chances of developing problems.
Smoking is the biggest troublemaker we see. It increases your risk of chronic periodontitis by 5 to 20 times compared to non-smokers. About 62% of current smokers aged 30 and older have periodontitis. Smoking reduces blood flow to your gums, making it harder for your body to fight infection.
Diabetes creates a particularly challenging situation because it has a two-way relationship with periodontal disease. High blood sugar makes you more susceptible to infections, while inflammation from periodontal disease makes it harder to control blood sugar levels. About 60% of adults with diabetes have periodontitis.
Hormonal changes can make your gums more sensitive to plaque bacteria. This is why many women notice their gums bleeding more during pregnancy, menstruation, or menopause.
Genetics play a bigger role than many people realize. Some families are simply more susceptible to severe gum disease, even with excellent oral hygiene.
Age matters too, with symptoms typically appearing in the 30s and 40s. By age 65, about 60% of adults have some form of periodontitis.
Medications can increase your risk by reducing saliva production or causing gum overgrowth, making it harder to keep teeth clean.
Stress weakens your immune system’s ability to fight off infections, including the bacteria that cause periodontal disease.
More info about What Factors Lead to Gum Disease?
Recognizing the Warning Signs
One of the most frustrating aspects of what is periodontal disease is that it’s often called a “silent” disease. Many patients don’t realize they have it until significant damage has occurred. However, your gums do give you warning signs if you know what to look for.
Red, swollen, or tender gums are often the first sign something’s wrong. Healthy gums should be pink and firm, not puffy or bright red. Bleeding gums during brushing, flossing, or even eating is never normal.
Persistent bad breath that doesn’t improve with brushing, mouthwash, or mints often indicates bacteria hiding in deep pockets around your teeth. Receding gums make your teeth appear longer and can expose sensitive root surfaces.
Loose or shifting teeth are serious warning signs that bone loss has progressed significantly. Pus between teeth and gums indicates active infection that needs immediate attention.
Painful chewing or increased tooth sensitivity can signal that the supporting structures around your teeth are compromised.
At PS Dental Services, I always tell patients not to ignore these warning signs. The earlier we catch periodontal disease, the more conservative and successful our treatment can be.
Diagnosis, Complications, Treatment & Prevention
Diagnosis
Diagnosing periodontal disease involves several key assessments that we perform during your comprehensive examination at PS Dental Services.
Periodontal probing is the gold standard for diagnosis. We use a thin, calibrated instrument called a periodontal probe to measure the depth of the space (pocket) between your gums and teeth. Healthy gum pockets measure 1-3 millimeters deep. Pockets deeper than 4mm indicate periodontal disease.
Dental X-rays reveal bone loss that isn’t visible during clinical examination. We can see the level of bone support around each tooth and identify areas where bone has been destroyed.
Medical and dental history helps us understand risk factors like smoking, diabetes, medications, and family history that might contribute to your condition.
Complications of Untreated Periodontal Disease
The consequences of untreated periodontal disease extend far beyond your mouth. Tooth loss is the most obvious complication – periodontitis and cavities are the two leading causes of tooth loss in adults.
Research has established links between periodontal disease and several systemic conditions:
Cardiovascular disease: Chronic inflammation from gum disease may contribute to heart disease, stroke, and high blood pressure.
Diabetes complications: Periodontal disease can make blood sugar control more difficult, while poorly controlled diabetes increases susceptibility to gum infections.
Pregnancy complications: Pregnant women with periodontal disease face higher risks of preterm birth and low birth weight babies.
Respiratory conditions: Bacteria from the mouth can be aspirated into the lungs, potentially contributing to pneumonia and other respiratory infections.
Research linking periodontal disease and diabetes
Treatment Options
The good news is that periodontal disease is treatable, and early intervention can prevent progression and restore health.
Non-surgical treatment is the first line of defense:
Scaling and root planing (deep cleaning) removes plaque and tartar from above and below the gum line. This procedure, performed under local anesthesia, smooths root surfaces to help gums reattach to teeth.
Local antimicrobials like chlorhexidine chips or antibiotic gels can be placed directly into periodontal pockets to target bacteria and reduce inflammation.
Oral antibiotics may be prescribed for aggressive or widespread infections.
Laser therapy offers a less invasive option for some patients, using focused light energy to remove infected tissue and bacteria.
Surgical treatment becomes necessary for advanced cases:
Flap surgery (pocket reduction surgery) allows direct access to root surfaces for thorough cleaning and may involve reshaping bone and gum tissue.
Bone grafting can help regenerate bone lost to periodontal disease using natural or synthetic materials.
Gum grafting addresses severe gum recession by transplanting tissue to cover exposed roots.
Guided tissue regeneration uses special membranes to direct new bone and tissue growth.
Platelet-rich fibrin (PRF) and platelet-rich plasma (PRP) therapies use your own blood components to accelerate healing and tissue regeneration.
More info about Periodontal Disease Treatment
Prevention Strategies
Prevention remains the most effective approach to periodontal disease. At PS Dental Services, we emphasize that preventing gum disease is much easier and less expensive than treating it.
Daily oral hygiene forms the foundation:
– Brush twice daily for two minutes with fluoride toothpaste
– Floss daily to remove plaque between teeth where brushes can’t reach
– Consider using an antimicrobial mouthwash
– Clean your tongue to reduce bacteria
Professional care is essential:
– Schedule dental cleanings every 6 months (or more frequently if recommended)
– Maintain regular dental checkups for early detection
– Follow through with recommended treatments promptly
Lifestyle modifications significantly impact your risk:
– Quit smoking or using tobacco products
– Manage diabetes effectively with your physician
– Maintain a balanced, nutritious diet
– Manage stress through healthy coping mechanisms
– Stay hydrated to maintain adequate saliva flow
Maintenance and Long-term Care
Once periodontal disease has been treated, lifelong maintenance becomes crucial. This typically involves:
Supportive periodontal therapy every 3-6 months, which includes professional cleaning, pocket depth monitoring, and assessment of disease stability.
Home care compliance with daily brushing, flossing, and any prescribed oral care products.
Regular monitoring of systemic health conditions that affect periodontal health.
Frequently Asked Questions about Periodontal Disease
Is periodontal disease curable or reversible?
This question comes up in nearly every conversation I have with patients about what is periodontal disease and their treatment options.
Gingivitis is your golden opportunity – it’s completely reversible when we catch it early. I’ve seen countless patients transform their gum health within just a few weeks of proper treatment and improved home care. Those red, swollen, bleeding gums can return to healthy pink tissue that doesn’t bleed when you brush or floss.
Periodontitis tells a different story. Once the infection has moved below the gum line and begun destroying bone and connective tissue, we enter management mode rather than cure mode. Think of it like other chronic conditions – diabetes, high blood pressure, or arthritis. With proper care and ongoing attention, you can live comfortably and healthily, but the condition requires lifelong management.
The reality is that bone and tissue that’s been lost typically doesn’t regenerate completely on its own. However, we can stop the disease progression, reduce inflammation, and often achieve remarkable improvements in comfort and function. Some newer regenerative treatments using your body’s own healing factors can help rebuild some lost support.
Your genetics play a role too. Some patients have inherited factors that make them more susceptible to gum disease, requiring more frequent maintenance visits and intensive home care.
The key takeaway? Early detection and treatment make all the difference. The sooner we address periodontal disease, the more we can preserve and the better your long-term outcomes will be.
Scientific research on periodontal therapy outcomes
Can periodontal disease affect my overall health?
This connection between your mouth and the rest of your body represents one of the most significant shifts in how we understand what is periodontal disease and its impact on your life. Your mouth isn’t an isolated system – it’s intimately connected to your entire body through your bloodstream and immune system.
Your heart feels the effects of chronic gum inflammation. While we can’t definitively say gum disease directly causes heart attacks, the research shows troubling connections. The same inflammatory processes damaging your gums may contribute to hardening of your arteries.
Diabetes creates a particularly challenging cycle. When your gums are chronically infected and inflamed, controlling blood sugar becomes more difficult. Meanwhile, liftd blood sugar levels make you more susceptible to infections, including gum disease. I work closely with patients’ physicians to break this cycle.
Pregnancy brings special concerns that many expectant mothers don’t realize. The inflammatory chemicals produced by diseased gums can potentially trigger early labor contractions. Studies suggest that pregnant women with periodontal disease face increased risks of preterm birth and having babies with low birth weight.
Your lungs can be affected when oral bacteria are breathed into the respiratory system. This becomes particularly worrisome for older adults or anyone with compromised immunity.
Even conditions like rheumatoid arthritis show interesting overlaps with periodontal disease, since both involve similar inflammatory pathways in the body.
The encouraging news is that treating periodontal disease often leads to improvements in these related health conditions.
When should I see a dentist for gum disease symptoms?
The short answer is don’t wait – schedule an appointment as soon as you notice any warning signs. I’ve seen too many patients who thought bleeding gums were normal or that bad breath would resolve on its own, only to find they had advanced periodontal disease that could have been easily managed if caught earlier.
Bleeding gums deserve immediate attention, despite the common misconception that this is normal. Healthy gums simply don’t bleed when you brush, floss, or eat an apple. If you’re seeing pink in the sink when you brush, call us within a week or two.
Persistent bad breath that doesn’t improve with brushing, flossing, or mouthwash often signals bacterial overgrowth below the gum line where your toothbrush can’t reach.
Changes in your gums like persistent redness, swelling, tenderness, or the appearance that your teeth are getting longer (gum recession) all warrant prompt evaluation. Loose teeth or changes in how your bite feels indicate more advanced disease that needs immediate professional attention.
Pain when chewing or increased tooth sensitivity may signal active infection that shouldn’t be ignored.
For patients with risk factors like diabetes, smoking history, or family history of gum disease, I often recommend checkups every 3-4 months instead of the standard six-month interval.
At PS Dental Services, we’d rather see you for a quick evaluation that reveals everything is fine than have you wait and find a small problem has become a major one.
More info about General Dentistry/Periodontal Therapy
Conclusion
Understanding what is periodontal disease is truly the foundation of protecting both your smile and your overall health. This surprisingly common condition affects millions of people, yet with the right knowledge and care, it’s largely preventable.
Think of your journey with gum health as a partnership between you and your dental team. At PS Dental Services in Tigard, Oregon, we’ve spent over 30 years helping families steer this journey, and we’ve learned that informed patients make the best decisions about their oral health.
The most important thing to remember is that gingivitis is completely reversible, while periodontitis is manageable with proper care. This means that catching problems early makes all the difference in the world.
What makes periodontal disease particularly tricky is its connection to your overall health. The inflammation in your mouth doesn’t stay in your mouth – it can affect your heart, your diabetes control, and even pregnancy outcomes. This is why Dr. Sepehri and our team view gum health as an essential part of your total wellness.
Modern treatment options give us incredible tools to help even patients with advanced periodontitis. From laser therapy to regenerative treatments using your own blood components, we can often achieve results that seemed impossible just a few years ago. But prevention through good daily care and regular professional cleanings remains your most powerful weapon.
Your gum health is definitely a lifelong journey rather than a one-time fix. With consistent daily brushing and flossing, regular professional care, and prompt attention to any changes, you can maintain healthy gums for decades to come.
Don’t wait for symptoms to get worse. If you’ve noticed bleeding gums, persistent bad breath, or any other warning signs, schedule an appointment soon. Early action today can prevent complex treatments down the road.
We encourage you to think of us as your partners in this journey. Whether you’re dealing with early signs of gum disease or need advanced treatment, we’re here to guide you through every step with compassion and expertise.
More info about periodontal therapy guide
Contact PS Dental Services today to schedule your comprehensive periodontal assessment. Your smile – and your whole body – will benefit from taking this important step toward optimal gum health.
Dr. Parisa Sepehri
Latest posts by Dr. Parisa Sepehri (see all)
- Mastering Dental Checkups: The Ultimate Guide to Cavity Treatment and General Dentistry for Preventive Care - September 15, 2025
- Transform Your Smile: The Top Benefits of a Hollywood Smile Makeover - September 14, 2025
- Unlocking the Power of Oral Appliance Therapy: A CPAP Alternative for Obstructive Sleep Apnea - September 13, 2025
- Unlocking the Benefits of Inpatient Dental Care: Special Needs Dentistry, Hospital Dentistry, and More! - September 12, 2025
- Revolutionizing Tooth Restoration: The Power of CEREC Crowns in Digital Dentistry - September 11, 2025